
Bariatric Surgery (Obesity Surgery)
- 13 Eylül 2019
- 17 Likes
- 826 Views
- 0 Comments
What is Obesity?
People with a body mass index of 30 and above are considered obese. It is calculated by dividing body weight by the square of height (kg/m²). It cannot be said that everyone with a body mass index over 30 will undergo surgery. In losing weight, healthy eating, diet and exercise methods should be tried first. If all preoperative interventions fail and future
– Some types of cancer (Breast, endometrial and prostate cancer),
– Increased risk of heart attack
– Paralysis,
– Hypertension,
– High cholesterol levels,
– Non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH),
– Sleep apnea,
– Type 2 diabetes,
If it is predicted that it may cause diseases, surgical intervention is required. Of course, what is important here is not the aesthetic expectations of the patient, but the medical opinion of the physician. The physician makes his decision after completing many intensive and complex medical procedures.
”The most dangerous element in Obesity Surgery is the misdirection of the patient. Unfortunately, with the information spread on social media and similar platforms, surgical intervention is described as a miracle. It should not be forgotten that before and after every surgical operation is as important as the surgery itself. Throughout this process, the patient has to be more careful about many issues, from eating habits to lifestyle.”
Obesity Surgery Methods:
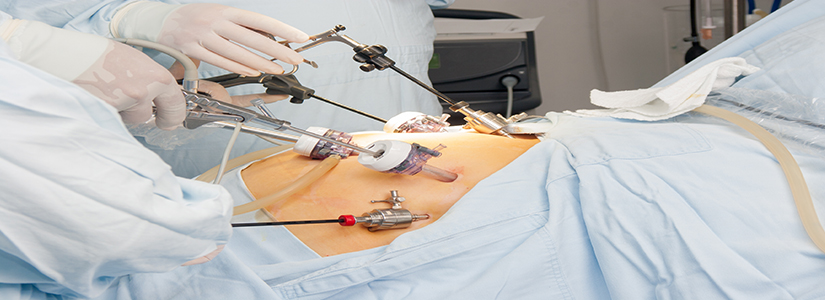
1. Laparoscopic (minimally invasive method) Surgery; Laparoscopy, which was used in the surgery of gynecological diseases in the past, is also used in gallbladder, hernia, spleen, liver, stomach and intestine surgeries with the developing technology. In traditional open surgery, an incision (port) covering the entire abdomen was required to reach the inside of the abdomen. In laparoscopic surgery, surgeries can be completed with a few incisions (ports) of 0.5-1 cm in size. Cannulas that are entered into the abdomen through the ports are called trocars. The surgeries are completed by advancing the camera through the trocars to see inside the abdomen and many tools specially developed for the laparoscopic technique. In the laparoscopic technique, the inside of the abdomen is inflated with carbon dioxide gas. In this way, the intra-abdominal organs move away from each other and space is obtained to perform surgery. Images from the camera are transferred to the operating room by high-resolution video monitors. During the surgery, the surgeon watches the images coming from inside the abdomen on the monitor. This system allows the surgeon to perform many surgeries with much smaller incisions than traditional methods. Advantages; Patients experience less pain compared to traditional open surgery. Faster recovery and shorter hospital stay. In addition, surgery completed through small incisions (Ports) has better cosmetic results. Is it safe? Laparoscopic technique is as safe as open surgery. The reason why laparoscopy is so safe is based on the experience of the performing surgeon. Many intestinal surgeries may have anesthesia-related (though much less frequent) bleeding and infectious complications. This risk depends on the nature of the disease. In addition, the patient’s health status and general performance may cause complications. Before any surgery you should discuss any possible risks with your surgeon.
5. Mini Gastric Bypass; This surgery consists of two surgical techniques. In the first stage, the most restrictive effect is observed by reducing the stomach volume to a smaller size than the gastric sleeve. In the second stage, 150-200 cm from the beginning of the small intestine is counted and the small intestine is combined with the newly created small stomach. Thus, we see the absorption-limiting effect in this surgical technique. While the patient experiences regular and sufficient weight loss after the surgery, it is an effective technique preferred in diseases caused by excessive weight gain (metabolic diseases such as Type 2 diabetes, high cholesterol and blood pressure).
6. Roux-Y Gastric Bypass; It is a commonly performed malabsorptive obesity surgery. Stomach volume is reduced and absorption is restricted. The weight loss rates achieved between mini gastric bypass and Roux -y gastric bypass are almost at the same level. Approximately from the point where the stomach meets the esophagus, a pouch of approximately 30-40 cc is created. Then, 50-70 cm from the first part of the small intestine is cut. The cut section is anastomosed to the newly created gastric pouch. On the other hand, it is connected to the other cut end, counting 150 cm from the anastomosis. It enables 70-80% loss of excess weight. Its effect on diabetes is around 80%. Since absorption is restricted, mineral and vitamin support is required.
* Anastomosis to Antrum; In surgeries performed for the treatment of the disease, hollow organs are stitched together to ensure the continuity of the organs. For example; The ends of the intestines left behind after intestinal surgery are stitched together to ensure continuity.
** Pouch; It acts as a reservoir to reduce the number of stools. This surgery eliminates the risk of recurrence of ulcerative colitis and allows normal defecation.



Leave Your Comment